Opening Times | Register | Contact Us
CQC Rating Good
Your Guide to Cervical Screening at Lakeside Surgery
Introduction
Due to COVID-19, there have been delays to the vital Cervical Screening service. You may have had to wait longer for your screening test or a follow-up appointment. However, the screening process is now back to normal, and there have been many patients who have not attended or delayed their smear.
In order to try and improve the screening service at Lakeside Surgery, we asked YOU what some of the reasons are for not attending or delaying your smear through a survey.
In response to the question “which of following are reasons why you have delayed/not attended cervical screening”:
- 30% ticked “I kept putting it off/did not get around to it.”
- 21% ticked “I found it hard to book an appointment at a convenient time.”
- 13% ticked “I was worried it would be painful or daunting.”
In response to the question “which of the following would make you more likely to book an appointment”:
- 23% ticked “More detailed explanations of what the risks are if I don’t have screening.”
- 20% ticked “I would like more information about the test and what the smear entails.”
This is a guide on Cervical Screening for everyone aged 25+ with a cervix at Lakeside Surgery.
So, what exactly is cervical screening?
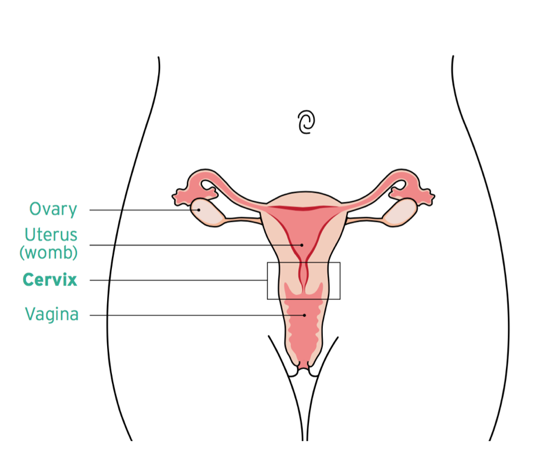
- Cervical screening (or a smear test) checks the health of your cervix. The cervix is the opening to your uterus from your vagina.
- Screening is a way of preventing cervical cancer.
What is cervical cancer?
- Cervical cancer occurs when the cells in the cervix grow in an uncontrolled way. As these cells grow, they can spread to the other parts of the body and become life threatening.
What is cervical cancer?
- Cervical cancer occurs when the cells in the cervix grow in an uncontrolled way. As these cells grow, they can spread to the other parts of the body and become life threatening.
What causes cervical cancer?
- Nearly all cervical cancers are caused by a virus called human papillomavirus (or HPV) – only 56% of responders to the survey knew this.
- HPV is a very common virus. It can be passed on through any type of sexual activity with a man or woman.
- Most men and women — about 80% of sexually active people in the UK — are infected with HPV at some point in their lives, but most people never know they have the virus.
- In most cases, your immune system can get rid of the virus without you ever knowing you had it.
- But sometimes, HPV infections can cause cells in your cervix to become abnormal.
- There are many different types of HPV, but only some of them can lead to cancer.
What are the benefits of cervical screening?
- Since the NHS Cervical Screening Programme was introduced in 1988, the number of women getting cervical cancer in England has gone down from over 4100 a year to 2300 a year in 2010.
- Cervical screening saves as many 5000 lives from cancer per year in the UK.
Who can have this screening?
- Everyone with a cervix aged 25 to 64 will be invited by letter or text.
When will I be invited?
This table below explains the current system in the UK.
| Age | When you're invited |
|---|---|
| Under 25 | up to 6 months before you turn 25 |
| 25 to 49 | every 3 years |
| 50 to 64 | every 5 years |
| 60 or older | only if 1 of you last 3 tests was abnormal |
If you're under 25
You will not be invited for cervical screening until you're 25 because:
- Cervical cancer is very rare in people under 25.
- It might lead to having treatment you do not need – abnormal cell changes often go back to normal in younger women.
- Researchers have worked out that screening younger women can lead to more harm than benefit.
However, if you develop symptoms that are you are worried about, you should book an appointment with your GP. Symptoms of cervical cancer are discussed further on.
If you’re 65 or older
- You’ll usually stop being invited for screening once you turn 65. This is because it is very unlikely that you will get cervical cancer.
- You will only be invited again if 1 of your last 3 smears was abnormal.
- If you're 65 or older and have never been for cervical screening or have not had cervical screening since the age of 50, you can ask your GP for a test.
If you have had a total hysterectomy
- You will not need to go for cervical screening if you have had a total hysterectomy to remove all of your womb and cervix.
If you are pregnant or just had a baby
- You will usually not need to have cervical screening if you are pregnant, or could be pregnant, until at least 12 weeks after you have given birth.
- This is because pregnancy can make it harder to get clear results.
- You will usually be advised to reschedule the test for a date around 12 weeks after your baby is born.
- If you've previously had an abnormal result from a cervical screening test, you may need to be screened while you're pregnant. Speak to your GP or midwife.
How do I book my appointment?
- 31.2% of the responders to the survey said they want “Reduced waiting time to book an appointment” (as the queues after calling reception are too long).
- However, there is no need to call reception.
- Our team at Lakeside are currently sending texts to those eligible or that have delayed screening in batches, with a link to a booking form.
- From April 2022 we will be sending out texts to all patients due smears on a monthly basis. Everyone that has a mobile number will receive the text - those without will be sent letters.
- We have found this is a very efficient method as it saves patients from calling into the surgery.
"The link I got last time took me straight to a booking form and I didn't have to remember my password"
Survey Responder
How do I prepare for my screening?
- Your appointment should be on a day when you are not on your period. If you don’t have periods, you can be screened at any time.
- Wearing a loose skirt (rather than trousers or a tight skirt) might make it easier to get ready for the test.
- Please don’t use any vaginal medications, lubricant or creams in the 2 days before you have your test because they can affect the sample your nurse or doctor takes.
What happens at the screening?
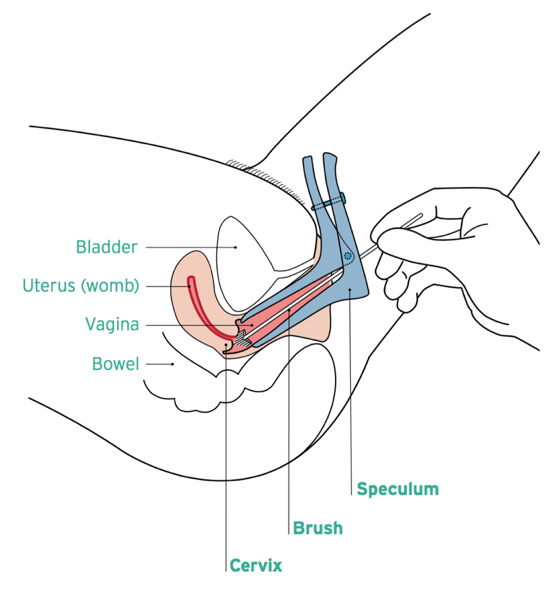
- The nurse or doctor will ask you to undress from your waist down and lie on a bed with your knees bent and apart.
- A device called a speculum will be put into your vagina and then used to open it gently. This allows the nurse or doctor to see your cervix.
- The sample is checked for certain types of human papillomavirus (HPV) that can cause changes to the cells of your cervix. These are called "high risk" types of HPV.
- If these types of HPV are not found, you do not need any further tests.
- If these types of HPV are found, the sample is then checked for any changes in the cells of your cervix. These can then be treated before they get a chance to turn into cervical cancer.
- The actual test takes only a minute or two. The whole appointment usually takes about 10 minutes.
- You'll get your results 2 weeks after your test.
What do my results mean?
Human papillomavirus (HPV) is not found in your sample
- Most people will not have HPV (HPV negative result).
- This means your risk of getting cervical cancer is very low. You do not need any further tests to check for abnormal cervical cells, even if you have had these in the past.
- You'll be invited for screening again in 3 or 5 years, depending on your age.
HPV is found in your sample
- Your results letter will explain what will happen next if HPV is found in your sample (HPV positive result).
- You may need:
- Another cervical screening test in 1 year
- A different test to look at your cervix (a colposcopy)
There are two different kinds of HV positive result:
| Result | What it means |
|---|---|
| HPV found (HPV positive) but no abnormal cells | You'll be invited for screening in 1 year and again in 2 years if you still have HPV. If you still have HPV after 3 years, you may need to have a colposcopy (a procedure to take a closer look at your cervix). |
| HPV found (HPV positive) and abnormal cells | You'll be asked to have a colposcopy. |
What are the symptoms of cervical cancer?
- Cervical cancer can have no symptoms, which is why screening is important.
- It can also develop between your regular screening.
- Therefore, it is important to look out for anything that is unusual for you, especially the following:
- Bleeding between your periods, after sex, or after the menopause.
- Abnormal vaginal discharge.
- Pain or discomfort during sex.
- If you have any of these changes, see a doctor as soon as possible. Don’t wait for your next cervical screening appointment.
- Usually these symptoms won’t mean you have cancer, but if you are found to have abnormal cells, you can get it diagnosed and treated early.
Are staff following the Covid rules during the screening process?
- 22% of responders to the survey wanted to ensure that “Staff are following the COVID rules - wearing gloves/masks/aprons and adequate cleaning measures are in place.”
- At Lakeside, all staff follow strict guidance on infection control to protect you and themselves.
- Staff ensure that they wear full PPE, and the couch is cleaned thoroughly in between patients.
- To protect yourself and staff members, please ensure you are also wearing a mask at all times.
What if I have had previous trauma or have certain conditions that makes it difficult for me to attend the screening?
- For many people, delaying cervical screening is a bit more complex than being shy or embarrassed. If you are a survivor of sexual violence, it can be a frightening and potentially triggering experience to put yourself in.
- If you suffer from conditions like vaginismus, vulvodynia or endometriosis where you feel pain in the vulva or vagina, booking the appointment could bring up extreme fear of potential pain.
- You may have also had a painful experience in the past, or suffer from mental health conditions.
- So, it’s not as easy as saying “get over it.”
"I have endometriosis. My 1st smear was extremely painful. I have yet to be invited for another one, but my first was enough to make me worry about another. An option of numbing/pain relief would take this fear away"
Survey Responder
Here are some tips for having a smear test on your own terms, staying in control and minimising fear/discomfort
- During a smear test, YOU are in control. If it hurts at any point, ask the nurse or doctor to stop.
- Let the practitioner know what your issues are, whether they are trauma, pain or anxiety related. If they know beforehand, they can suggest ways to lessen any pain.
- If you can, try and organise someone you trust to take you to your appointment and back home.
- You can take a mild painkiller like paracetamol or ibuprofen 30 minutes before your appointment if you are worried about any pain.
- Before your appointment, ask for a spare speculum to take home and practise with. You can ask your GP or whoever you are booking an appointment with. This will help you get used to the feeling of penetration if that’s an issue for you, and the feeling of the speculum opening, all in the comfort of your own home.
- If for any reason you cannot get hold of a speculum, take some time to practise gentle penetration and stretching of the tissue with your own clean fingers.
- You can also ask to insert the speculum yourself. The practitioner will be more than happy to allow this and will also guide you if you need it.
- Ask for a smaller speculum. Speculums come in different sizes, so you can ask your practitioner to use a smaller size.
- If you have vaginal dryness, you can ask the practitioner to give you a vaginal oestrogen cream, pessary or more lube. This can make inserting the speculum easier.
- Ask the practitioner to ask you before each step of the process if it’s okay to continue, and to describe what they’re about to do before each step. This may be particularly useful for someone who has had their consent violated in the past.
- Practise breathing exercises beforehand. There are plenty on YouTube.
- Take a podcast, music or a meditation app to listen to - this may help you relax or distract you.
- Organise a treat for after your appointment, like cake and coffee at a café, to distract you and give you something to look forward to.
Finally remember
- You can stop at any moment and rebook your appointment. Do not push yourself or your body if you are feeling deeply distressed by the experience. It is not a failure to take a step back and try again.
- There are several resources at the end that can further help you.
Your comments from the survey
I would like the cervical screening check not just for HPV but also to check the cell morphology, even if the HPV test result is negative
- As you may be aware, the UK has moved to HPV primary testing (or screening) in the cervical screening programme.
- The sample taken will be tested for HPV first, rather than for cell changes first.
- You might be wondering why this has changed. HPV causes 99.7% of cervical cancers, so testing for HPV means we can identify who is most at risk of developing cell changes or cervical cancer. This means we can give the right people the care they need as early as possible.
- More than 15 years of research has produced a strong evidence base supporting HPV testing compared to cytology testing.
- This is why several countries are now updating their screening guidelines.
- It is incredibly rare to have cervical cancer without HPV. If HPV is present, then we look at cells under the microscope.
- Anybody with abnormal cells is invited for a colposcopy for a closer look.
Cervical screening should be every 2 years
- Research has shown that for anyone who has had a negative HPV test, it is highly unlikely for them to develop cervical cancer within 3-5 years, which is why we do not screen patients before then.
I had panic attacks during my last smear, and now I am too scared of that happening again. Self-sampling at home would be the best development for me.
- Firstly, we are incredibly sorry to hear anyone having a bad experience with previous smears. Please read the detailed section above on how to help make the screening process easier for you.
- 10% of responders from the survey would also like the option of a self-sample kit at home. This could potentially revolutionise the screening system.
- More than 31,000 women were part of a study conducted in London in 2021, where they were sent self-sample kits for HPV at home.
- While we would like everyone to have access to self-sampling, this is a study running in North and East London. Hopefully the results of the study will mean that anyone who wishes to will soon able to have the option to use a self-sample.
- While self-sampling kits are currently available to purchase privately, they are not part of the NHS cervical screening programme and studies such as this one are essential to ensure they are introduced in the safest and most effective way.
Further Resources
- Video Series explaining Cervical Screening at Lakeside Surgery – Dr Devyani Shete
- The NHS Cervical Screening Programme
- Informed Choice about Cancer Screening
- Cancer Research UK
- Jo’s Cervical Cancer Trust
- Help after sexual assault
- Living with vaginismum
- Talking therapy services for mental health or sexual assault
We use cookies to help provide you with the best possible online experience.
By using this site, you agree that we may store and access cookies on your device. Cookie policy.
Cookie settings.
Functional Cookies
Functional Cookies are enabled by default at all times so that we can save your preferences for cookie settings and ensure site works and delivers best experience.
3rd Party Cookies
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
